Anti-Brucella abortus ELISA (IgG)
| ORDER NO. | ANTIBODIES AGAINST | IG-CLASS | SUBSTRATE | FORMAT |
|---|---|---|---|---|
| EI 2189-9601 G | Brucella abortus | IgM | Ag-coated microplate wells | 96 x 01 (96) |
Indication: The ELISA test kit provides a semiquantitative or quantitative in vitro assay for human antibodies of the immunoglobulin class IgG class against Brucella abortus in serum or plasma for the diagnosis of brucellosis.
Application: The Anti-Brucella abortus ELISA is a supplement to the direct pathogen detection for the diagnosis of Brucellosis. Taking into consideration the clinical symptoms, detection of IgM and/or IgA antibodies and a clear titer increase of IgG antibodies in a serum pair taken after at least 2 weeks time can be seen as indication for an acute Brucella infection. Moreover, serological investigations are suitable for clarification of epidemiological questions.
Principle of the test: The test kit contains microtiter strips each with 8 break-off reagent wells coated with Brucella abortus antigens. In the first reaction step, diluted patient samples are incubated in the wells. In the case of positive samples, specific IgG (also IgA and IgM) antibodies will bind to the antigens. To detect the bound antibodies, a second incubation is carried out using an enzyme-labelled anti-human IgG (enzyme conjugate) catalysing a colour reaction.
| Component | Colour | Format | Symbol |
|---|---|---|---|
| 1. Microplate wells coated with antigens 12 microplate strips each containing 8 individual break-off wells in a frame, ready for use | --- | 12 x 8 | STRIPS |
| 2. Calibrator 1 200 RU/ml (IgG, human), ready for use | dark red | 1 x 2.0 ml | CAL1 |
| 3. Calibrator 2 20 RU/ml (IgG, human), ready for use | red | 1 x 2.0 ml | CAL2 |
| 4. Calibrator 3 2 RU/ml, (IgG, human), ready for use | light red | 1 x 2.0 ml | CAL3 |
| 5. Positive control (IgG, human), ready for use | blue | 1 x 2.0 ml | POS CONTROL |
| 6. Negative control (IgG, human), ready for use | green | 1 x 2.0 ml | NEG CONTROL |
| 7. Enzyme conjugate peroxidase-labelled anti-human IgG (rabbit), ready for use | green | 1 x 12 ml | CONJUGATE |
| 8. Sample buffer ready for use | light blue | 1 x 100 ml | SAMPLE BUFFER |
| 9. Wash buffer 10x concentrate | colourless | 1 x 100 ml | WASH BUFFER 10x |
| 10. Chromogen/substrate solution TMB/H2O2, ready for use | colourless | 1 x 12 ml | SUBSTRATE |
| 11. Stop solution 0.5 M sulphuric acid, ready for use | colourless | 1 x 12 ml | STOP SOLUTION |
| 12. Test instruction | --- | 1 booklet | |
| 13. Quality control certificate | --- | 1 protocol |
Preparation and stability of the reagents
Note: All reagents must be brought to room temperature (+18°C to +25°C) approx. 30 minutes before use. After first use, the reagents are stable until the indicated expiry date if stored at +2°C to +8°C and protected from contamination, unless stated otherwise below.
- Coated wells: Ready for use. Tear open the resealable protective wrapping of the microplate at the recesses above the grip seam. Do not open until the microplate has reached room temperature to prevent the individual strips from moistening. Immediately replace the remaining wells of a partly used microplate in the protective wrapping and tightly seal with the integrated grip seam (Do not remove the desiccant bag). Once the protective wrapping has been opened for the first time, the wells coated with antigens can be stored in a dry place and at a temperature between +2°C and +8°C for 4 months.
- Calibrators and controls: Ready for use. The reagents must be mixed thoroughly before use.
- Enzyme conjugate: Ready for use. The enzyme conjugate must be mixed thoroughly before use.
- Sample buffer: Ready for use.
- Wash buffer: The wash buffer is a 10x concentrate. If crystallisation occurs in the concentrated buffer, warm it to +37°C and mix well before diluting. The quantity required should be removed from the bottle using a clean pipette and diluted with deionised or distilled water (1 part reagent plus 9 parts distilled water). For example: For 1 microplate strip, 5 ml concentrate plus 45 ml water. The working strength wash buffer is stable for 4 weeks when stored at +2°C to +8°C and handled properly.
- Chromogen/substrate solution: Ready for use. Close the bottle immediately after use, as the contents are sensitive to light . The chromogen/substrate solution must be clear on use. Do not use the solution if it is blue coloured.
- Stop solution: Ready for use.
Storage and stability: The test kit has to be stored at a temperature between +2°C to +8°C. Do not freeze. Unopened, all test kit components are stable until the indicated expiry date.
Waste disposal: Patient samples, calibrators, controls and incubated microplate strips should be handled as infectious waste. All reagents are to be disposed of according to official regulations.
Warning: The calibrators and controls of human origin have tested negative for HBsAg, anti-HCV, anti- HIV-1 and anti-HIV-2. Nonetheless, all materials should be treated as being a potential infection hazard and should be handled with care. Some of the reagents contain sodium azide in a non-declarable concentration. Avoid skin contact.
Preparation and stability of the patient samples
Sample: Human serum or EDTA, heparin or citrate plasma.
Stability: Patient samples to be investigated can generally be stored at +2°C to +8°C for up to 14 days. Diluted samples should be incubated within one working day.
Sample dilution: Patient samples are diluted 1:101 in sample buffer. For example: dilute 10 ?l sample to 1.0 ml sample buffer and mix well by vortexing (sample pipettes are not suitable for mixing).
NOTE: Calibrators and controls are prediluted and ready for use, do not dilute them.
Incubation
For semiquantative analysis incubate calibrator 2 along with the positive and negative controls and patient samples. For quantitative analysis incubate calibrators 1, 2 and 3 along with the positive and negative controls and patient samples.
| Sample incubation:(1st step) | Transfer 100 ?l of the calibrator, positive and negative controls or diluted patient samples into the individual microplate wells according to the pipetting protocol. Incubate for 30 minutes at room temperature (+18°C to +25°C). |
|---|---|
| Washing: | Manual: Empty the wells and subsequently wash 3 times using 300 ?l of working strength wash buffer for each wash. Automatic: Wash the reagent wells 3 times with 450 ?l of working strength wash buffer (program setting: e.g. TECAN Columbus Washer “Overflow Mode”). Leave the wash buffer in each well for 30 to 60 seconds per washing cycle, then empty the wells. After washing (manual and automated tests), thoroughly dispose of all liquid from the microplate by tapping it on absorbent paper with the openings facing downwards to remove all residual wash buffer. Note: Residual liquid (> 10 ?l) in the reagent wells after washing can interfere with the substrate and lead to false low extinction readings. Insufficient washing (e.g., less than 3 wash cycles, too small wash buffer volumes, or too short residence times) can lead to false high extinction readings. Free positions on the microplate strip should be filled with blank wells of the same plate format as that of the parameter to be investigated. |
| Conjugate incubation:(2nd step) | Pipette 100 ?l of enzyme conjugate (peroxidase-labelled anti-human IgG) into each of the microplate wells. Incubate for 30 minutes at room temperature (+18°C to +25°C). |
| Washing: | Empty the wells. Wash as described above. |
| Substrate incubation:(3rd step) | Pipette 100 ?l of chromogen/substrate solution into each of the microplate wells. Incubate for 15 minutes at room temperature (+18°C to 25°C) (protect from direct sunlight). |
| Stopping: | Pipette 100 ?l of stop solution into each of the microplate wells in the same order and at the same speed as the chromogen/substrate solution was introduced. |
| Measurement: | Photometric measurement of the colour intensity should be made at a wavelength of 450 nm and a reference wavelength between 620 nm and 650 nm within 30 minutes of adding the stop solution. Prior to measuring, slightly shake the microplate to ensure a homogeneous distribution of the solution. |
Pipetting protocol
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| A | C 2 | P 6 | P 14 | P 22 | C 1 | P 4 | P 12 | P 20 | ||||
| B | pos. | P 7 | P 15 | P 23 | C 2 | P 5 | P 13 | P 21 | ||||
| C | neg. | P 8 | P 15 | P 23 | C 3 | P 6 | P 14 | P 22 | ||||
| D | P 1 | P 9 | P 17 | pos. | P 7 | P 15 | P 23 | |||||
| E | P 2 | P 10 | P 18 | neg. | P 8 | P 16 | P 24 | |||||
| F | P 3 | P 11 | P 19 | P 1 | P 9 | P 17 | ||||||
| G | P 4 | P 12 | P 20 | P 2 | P 10 | P 18 | ||||||
| H | P 5 | P 13 | P 21 | P 3 | P 11 | P 19 |
The pipetting protocol for microtiter strips 1 to 4 is an example for the semiquantitative analysis of 24 patient samples (P 1 to P 24). The pipetting protocol for microtiter strips 7 to 10 is an example for the quantitative analysis of 24 patient samples (P 1 to P 24).
The calibrators (C 1 to C 3), the positive (pos.) and negative (neg.) controls, and the patient samples have each been incubated in one well. The reliability of the ELISA test can be improved by duplicate determinations for each sample. The wells can be broken off individually from the strips. This makes it possible to adjust the number of test substrates used to the number of samples to be examined and minimizes reagent wastage. Both positive and negative controls serve as internal controls for the reliability of the test procedure. They should be assayed with each test run.
Calculation of results
Semiquantitative: Results can be evaluated semiquantitatively by calculating a ratio of the extinction of the control or patient sample over the extinction of the calibrator 2. Calculate the ratio according to the following formula:
| Extinction of the control or patient sample | |
|---|---|
| Extinction of calibrator 2 | = Ratio |
EUROIMMUN recommends interpreting results as follows:
| Ratio <0> | negative |
|---|---|
| Ratio ≥0.8 to <1> | borderline |
| Ratio ≥1.1: | positive |
Quantitative: The standard curve from which the concentration of antibodies in the patient samples can be taken is obtained by point-to-point plotting of the extinction reading measured for the 3 calibration sera against the corresponding units (linear/linear). Use “point-to-point” plotting for calculation of the standard curve by computer. The following plot is an example of a typical calibration curve. Please do not use this curve for the determination of antibody concentrations in patient samples.
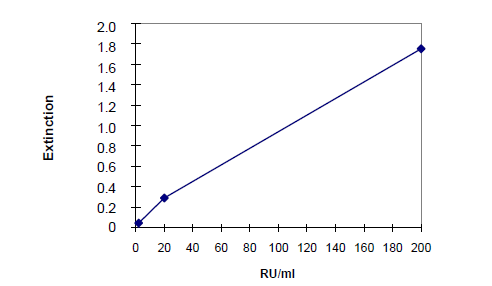
If the extinction for a patient sample lies above the value of calibrator 1 (200 RU/ml), the result should be reported as “>200 RU/ml”. It is recommended that the sample be retested at a dilution of e.g.1:400. The result in RU/ml read from the calibration curve for this sample must then be multiplied by a factor of 4.
The upper limit of the normal range of non-infected persons (cut-off value) recommended by EUROIMMUN is 20 relative units (RU)/ml. EUROIMMUN recommends interpreting results as follows:
| <16> | negative |
|---|---|
| ≥16 to <22> | borderline |
| ≥22 RU/ml: | positive |
For duplicate determinations the mean of the two values should be taken. If the two values deviate substantially from one another, EUROIMMUN recommends retesting the samples.
A negative serological result does not exclude an infection. Particularly in the early phase of an infection, antibodies may not yet be present or are only present in such small quantities that they are not detectable. In case of a borderline result, a secure evaluation is not possible. If there is a clinical suspicion and a negative test result, we recommend clarification by means of other diagnostic methods and/or the serological investigation of a follow-up sample. A positive result indicates that there has been contact with the pathogen. In the determination of pathogen-specific IgM antibodies, polyclonal stimulation of the immune system or antibody persistence may affect the diagnostic relevance of positive findings. Significant IgG titer increases (exceeding factor 2) and/or seroconversion in a follow-up sample taken after at least 7 to 10 days can indicate an acute infection. To investigate titer changes, sample and follow-up sample should be incubated in adjacent wells of the ELISA microplate within the same test run. For diagnosis, the clinical picture of the patient always needs to be taken into account along with the serological findings.
Test characteristics
Calibration: As no quantificated international reference serum exists for antibodies against Brucella abortus, the calibration is performed in relative units (RU). For every group of tests performed, the extinction readings of the calibrators and the relative units and/or ratios determined for the positive and negative controls must lie within the limits stated for the relevant test kit lot. A quality control certificate containing these reference values is included. If the values specified for the controls are not achieved, the test results may be inaccurate and the test should be repeated. The binding activity of the antibodies and the activity of the enzyme used are temperature-dependent. It is therefore recommended using a thermostat in all three incubation steps. The higher the room temperature (+18°C to +25°C) during the incubation steps, the greater will be the extinction. Corresponding variations apply also to the incubation times. However, the calibrators subject to the same influences, with the result that such variations will be largely compensated in the calculation of the result.
Antigen: The antigen used is Brucella abortus of strain W99.
Linearity: The linearity of the Anti-Brucella abortus ELISA (IgG) was determined by assaying at least serial dilutions of patient sample with high antibody concentrations. The Anti-Brucella abortus ELISA (IgG) is linear at least in the tested concentration range 2 RU/ml to 200 RU/ml.
Detection limit: The lower detection limit is defined as the mean value of an analyte-free sample plus three times the standard deviation and is the smallest detectable antibody titer. The lower detection limit of the Anti-Brucella abortus ELISA (IgG) is 0.4 RU/ml.
Cross reactivity: The quality of the antigen (whole antigen) used and the antigen source (Brucella abortus strain W99) ensure a high specificity of the ELISA. An increased titer of antibodies against O-antigens of Yersinia enterocolitica 09, Francisella tularensis, Vibrio choleare, E. coli 0157, Stenotrophomonas maltophila and salmonellae can lead to false-positive results due to cross-reactions. With Vibrio cholerae cross-reactions may occur in infections as well as after immunisation.
| Antibodies against | n | Anti-Brucella abortus (IgG) positive |
|---|---|---|
| Salmonella | 11 | 0 % |
| Yersinia | 12 | 0 % |
Interference: No interference was observed with haemolytic, lipaemic or icteric samples for concentrations of up to 10 mg/ml for haemoglobin, 20 mg/ml for triglyceride and 0.4 mg/ml for bilirubin.
Reproducibility: The reproducibility of the test was investigated by determining the intra- and interassay coefficients of variation (CV) using 3 samples. The intra-assay CVs are based on 20 determinations and the inter-assay CVs on 4 determinations performed in 6 different test runs.
| Intra-assay variation, n = 20 | ||
|---|---|---|
| Sample | Mean value(RU/ml) | CV(%) |
| 1 | 31 | 8.8 |
| 3 | 80 | 3.1 |
| 2 | 111 | 4.7 |
| Inter-assay variation, n = 4 x 6 | ||
|---|---|---|
| Sample | Mean value(RU/ml) | CV(%) |
| 1 | 29 | 7.7 |
| 3 | 84 | 7.0 |
| 2 | 125 | 5.2 |
Sensitivity and specificity: 123 pre-characterised patient samples tested positive with the Rose-Bengal-Test (IgA, G, M) were examined with the Anti-Brucella abortus ELISA (IgA, IgG, IgM, respectively). For the determination of the specificity 160 blood donors were tested. Both groups originated from Turkey. The data yielded were as follows: Anti-Brucella abortus IgA: Sensitivity 88.8% at a specificity of 98.0%, Anti-Brucella abortus IgG: Sensitivity 78.2% at a specificity of 98.0% and Anti-Brucella abortus IgM: Sensitivity 56.1% at a specificity of 98.0%. The combined evaluation of all three immunoglobulin classes IgA, IgG and/or IgM results in an overall sensitivity of 98.3% with respect to the Rose-Bengal-Test.
Reference range: The levels of the antibodies against Brucella abortus (IgG) were analyzed with this EUROIMMUN ELISA in a panel of 282 healthy blood donors. With a Cut-off of 20 RU/ml, 0.4% of the blood donors were anti-Brucella abortus positive (IgG).
Clinical significance
Brucella abortus belongs to the genus Brucella and is the most frequent causative agent of brucellosis in the Western hemisphere. The pathogen is a gram-negative, aerobically growing, coccoidal, immobile (rod-shaped) bacterium which does not form spores. It is one of the four worldwide distributed Brucella species/biovars that are transmitted from infected animals to humans at close contact. Brucella abortus is found predominantly in cattle, while Brucella melitensis found in goats, camels and sheep, Brucella suis in pigs and Brucella canis in dogs.
These obligatory pathogens of zooanthroponosis cause acute or chronic general infections with fever and granulosmatous tissue reactions in humans. Worldwide, around 500,000 cases of brucellosis in humans are registered every year.
Brucella abortus, which was discovered in 1896 by the Danish bacteriologist Bernhard Lauritz Frederik Bang (1848-1932), can be found worldwide and is transmitted by direct contact with cattle or by consuming unpasteurised milk or dairy products or insufficiently cooked beef. Human to human transmission is rare but may occur in isolated cases through breast milk or sexual intercourse. Brucella abortus, the causative agent of brucellosis (Bang’s disease), can enter the human body via the gastrointestinal tract, the respiratory tract or skin wounds. There, the pathogen is first absorbed by polymorphonuclear granulocytes and later by macrophages and subsequently transported to the nearest lymph nodes. Brucella may also enter the bloodstream through the lymph system and spread haematogenously in organs that are rich in macrophages such as the spleen, liver, bone marrow and lungs. The testes, gall bladder, prostate and central nervous system can also be affected.
The disease manifests in various ways. The main forms of manifestation are the following:
- Subclinical brucellosis: Up to 90% of infections are subclinical infections. Diagnosis is only achieved by the determination of specific antibodies, which are the result of an effective humoral and cellular immune response of the host organism.
- Subacute to acute brucellosis After an incubation period of two weeks to several months, the onset of the infection is insidious, starting with fever, nausea, headache and joint pains, night sweat, weight loss and depressive mood. The fever continues for 7 to 21 days with afebrile intervals of 2 to 5 days (undulating fever). Clinical signs such as swelling of the lymph nodes, splenomegaly and hepatomegaly are rare.
- Chronic brucellosis: In cases of undetected infection or incorrect treatment, a longer course of the disease is not unusual. A brucellosis infection is considered as chronic when it persists for more than a year. In approximately 5% of patients the infection develops into a chronic form after the acute symptoms have disappeared. The disease manifests in unspecific general symptoms, e.g. lassitude, depression and sleeplessness. In addition to hepatosplenomegaly, 20 to 40% of patients experience complications, with bone and joint involvement (e.g. arthritis, bursitis), orchitis and meningitis. Affection of the bone marrow results in anaemia, leucopenia and thrombopenia.
In Germany, brucellosis is a notifiable disease according to the German law for the protection against infections (Infektionsschutzgesetz). The diagnosis of brucellosis is supplemented by serological methods. Agglutination tests are increasingly being replaced by antibody class specific ELISA (e.g. IgA, IgG and IgM Anti-Brucella abortus ELISA), which provide higher sensitivity and specificity (over 95%). Besides the determination of the antibody class, the measurement of titer level and titer increases is especially important for final diagnosis.
Acute, subacute and chronic brucellosis and brucellosis with involvement of the central nervous system can be differentiated by determining the antibody titer of Brucella specific IgA, IgM and IgG antibodies. In patients with acute brucellosis IgA (98%), IgG (97%) and IgM (100%) are detected, in subacute brucellosis IgA (100%), IgG (100%) and IgM (86%), in chronic brucellosis IgA (100%), IgG (100%) and IgM (33%) and in brucellosis with involvement of the central nervous system IgA (85%), IgG (100%) and IgM (20%). Cross reactions may occur with E. coli und Y. enterocolitica.
Additionally to the serological determination, Brucella abortus infections in cows can also be diagnosed by the detection of specific antibodies in their milk using ELISA, which shows a sensitivity of 98.5% and a specificity of 99.9%.
Brucellosis can be treated with antibiotics. A vaccine for humans has not yet been developed. Besides personal hygiene, successful preventive measures against brucellosis in humans include monitoring and elimination of infected live stock, burning of carcasses, regulation of imports and pasteurisation of milk.